Investigation and Treament of Facial Pain:
 Pain in the face may result from many different disorders and often presents as a diagnostic problem to the neurologist or neurosurgeon.
Pain in the face may result from many different disorders and often presents as a diagnostic problem to the neurologist or neurosurgeon.
Quality of pain
- Trigeminal neuralgia – sharp, stabbing, shooting, paroxysmal
- Atypical facial pain – dull, persisting
- Postherpetic neuralgia – dull, burning, persisting, occasional paroxysm
- Dental – dull
- Sinusitis – sharp, boring, worse in the morning
- Ocular – dull, throbbing
- Costen’s syndrome – severe aching, aggravated by chewing
- Cluster headache – sharp, intermittent
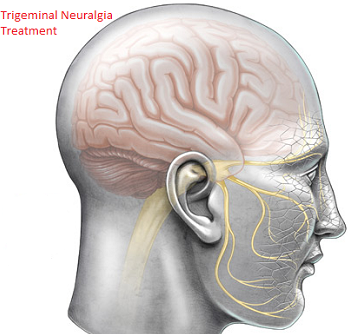
Trigeminal Neuralgia
Trigeminal neuralgia is characterised by paroxysmal attacks of severe, short, sharp, stabbing pain affecting one or more divisions of the trigeminal nerve. The pain involves the second or third divisions more often than the first; it rarely occurs bilaterally and never simultaneously on each side, occasionally more than one division is involved. Paroxysmal attacks last for several days or weeks; they are often superimposed on a more constant ache. When the attacks settle, the patient may remain pain free for many months.
Chewing, speaking, washing the face, tooth-brushing, cold winds, or touching a specific ‘trigger spot’, e.g. upper lip or gum, may all precipitate an attack of pain.
Trigeminal neuralgia more commonly affects females and patients over 50 years of age.
Aetiology
Trigeminal pain may be symptomatic of disorders which affect the nerve root or its entry zone
Root or root entry zone compression
- Arterial Vessels often abut and sometimes clearly indent the trigeminal nerve root at the entry-zone into the pons, causing ephaptic transmission (short circuiting).
- Tumours of the cerebellopontine angle lying against the V nerve roots, e.g. meningioma, epidermoid cyst, frequently present with trigeminal pain.
Demyelination – such a lesion in the pons should be considered in a ‘young’ person with trigeminal neuralgia. Trigger spots are rare. Remission occurs infrequently and the response to drug treatment is poor.
In some patients the cause remains unexplained, as do the long periods remission.
Investigation
MR scan to exclude a cerebello-pontine angle lesion or demyelination.
Results and complications
Pain relief- no comparative trials have been done so accurate comparison of the wide variety of techniques used for trigeminal neuralgia is difficult. Microvascular decompression seems to be more likely to provide pain control with fewer relapses. Overall 80-85% of patients remain pain free for a 5-year period. Results of peripheral nerve avulsion are less satisfactory with pain recurring in 5000 within 2 years.
- Dysaesthesia\Anaesthesia dolorosa – This troublesome sensory disturbance follows any destructive technique to nerve or root in 5-30% of patients. Microvascular decompression avoids this.
- Corneal anaesthesia – This occurs when root section or thermocoagulation involves the first division and keratitis may result.
- Mortality – Microvascular decompression and open root section carry a very low mortality (< 1%), but this must not be ignored when comparing results with safer methods.
Treatment selection: This depends on discussion of the differing risks with the patient. In younger patients the absences of sensory complications make microvascular decompression the procedure of first choice. Frail and elderly patients may tolerate glycerol injection, balloon compression and thermocoagulation more easily than other procedures.
Braner Clinics is a professional corporation, and was established for the practice of chronic pain management in 1990. Appointments are on a first come first serve basis. If you are going to miss your appointment please call at least 48 hours in advance, as there may be a waiting list. You may be asked for a credit card deposit for $25 towards your appointment. This deposit will be deducted from your first visit. If you miss your appointment this deposit will not be refunded to you.