Headache!!
According to recent studies, 45 millions of Americans suffer from chronic headaches. Charles Flippen, M.D., associate professor of Neurology at the David Giffen School of Medicine at UCLA states,”we know what areas of brain are generating pain but we don’t have the whole picture.” So to find appropriate treatment for your headache kind can be little bit difficult and to find the appropriate one, you need to identify the headache you are experiencing before it starts causing discomfort to you.
What do you mean by headache?
Any type of pain in head, neck or scalp can be identified as headache. Till today, 150 categories of diagnostic headaches with varying effects and causes have been set up.
Luckily, most of the headaches can be treated with the help and apt synthesis of pharmacology, environmental changes, stress management and certain changes in diet and lifestyle.
What are the major types of headaches?
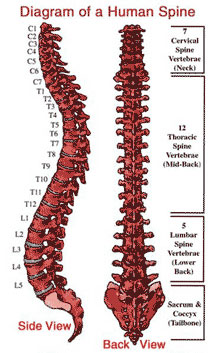
- Tension headaches: Tension Headaches, also referred to as ‘hat band’ headaches, cause pain around the back of head and neck, temples and forehead. It can last for few hours to several days. Tension in the neck, face and scalp muscles due to stress, anxiety, depression, hunger, exposure to caustic fumes, poor sleeping or sitting posture can trigger this type of headache. Over the counter medicines like; aspirin, ibuprofen or acetaminophen can treat these headaches.
- Migraine Headaches: It is the most common and debilitating type of headache causing pain usually (not always) at the one side of the head and often followed by vomiting or nausea, sensitivity to light, sound or odor. It lasts for 4 to 72 hours. Some patients may experience visual distortion or hand numbness due to migraines. Exact causes of migraine are till not known but genes play an important role. Doctors advice acupuncture, relaxation techniques, Vitamin B12 and Magnesium supplements and Triptan medications as the treatment options.
- Rebound Headaches or MOH (Medication Overuse Headaches): Experts are warning another new kind of headache especially among the severe headache sufferers known as rebound or medication overuse headaches. These headaches happen due to overuse of medications to treat headaches. Over the counter medications like; aspirin, acetaminophen, ibuprofen and other prescription drugs induce such headaches. Doctors advice to discontinue the use of such medicines, if they are triggering more headaches. Treatment for these headaches depends upon the patient and severity of his condition.
- Sinus Headaches: When sinus becomes inflamed due to infection or seasonal allergies, it, at times causes pain in the forehead, cheekbones and bridge of the nose. Such pain is usually accompanied by fever and green nasal discharge. Leaning forward or sudden head movement worsen such pain. Doctors recommend antibiotics and antihistamines for the treatment of these headaches.
- Cluster Headaches: Cluster Headaches are recurring headaches that occur in group or cycles and are characterized by ‘remission period’. In other words, headaches may disappear for months or years before recurring. These headaches cause throbbing pain on the one side of the head with watery eye and nasal congestion or stuffy nose on the same side. Patient feels restless during an attack and finds himself unable to settle down. There is no known medication or cure for treating cluster headaches, but medicines or magnesium infusion can reduce the frequency and duration of attacks.
- Dental or oral induced Headaches: Certain dental conditions like bruxism or temporomandibular joint disorder (TMJ) can also trigger headache. Such headaches are more severe in the morning after night of teeth grinding or during the stressful hours of the day. A person’s way of bite or teeth coming together can trigger such aches. Patients should visit dentists for ‘occlusion training.’ Treatments include; wearing specially fitted night guards, braces, veneers, stretching the jaw, hot or cold pack and stress reduction.
Do not delay your visit to your physician, if you are experiencing recurrent and throbbing headaches; as they may indicate a serious underlying problem. So any headache followed by neck stiffness, slurred speech or weakness should be consulted immediately before it becomes plaguing and life threatening.
Contact Braner Pain Clinics for the multidisciplinary management and appropriate treatment of your persistent chronic pain. We make use of cutting edge techniques and technologies to make your life pain free as well as hassle free.