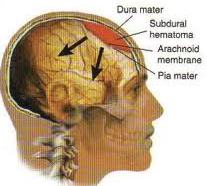
Risk Factors and Complications of Cerebral Aneurysms (Brain Injury):
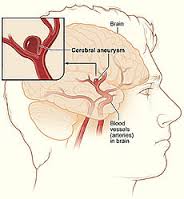 A Cerebral Aneurysm is a huge, weak area in the wall of an artery that supplies blood vessels to the mind. In most situations, a brain aneurysm causes no symptoms and goes unseen. In rare situations, the brain aneurysm bursts, launching blood vessels into the head and causing a heart stroke.
A Cerebral Aneurysm is a huge, weak area in the wall of an artery that supplies blood vessels to the mind. In most situations, a brain aneurysm causes no symptoms and goes unseen. In rare situations, the brain aneurysm bursts, launching blood vessels into the head and causing a heart stroke.
Risk Factors
- Atherosclerotic diseases
- Family history
- Polycystic Kidney Disease
Pathogenesis
The cause of aneurysm formation may be multifactorial with acquired factors combining with an underlying genetic susceptibility.
- Aneurysms were once thought to be ‘congenital’ due to the finding of developmental defects in the tunica media.
- Aneurysms often form at sites of haemodynamic stress where for example, a congenitally hypoplastic vessel leads to excessive flow in an adjacent artery.
- It is not known whether they form rapidly over the space of a few minutes, or more slowly over days, weeks, or months.
Clinical Presentation
Of those patients with intracranial aneurysms presenting acutely, most have had a subarachnoid haemorrhage. A few present with symptoms or signs due to compression of adjacent structures. Others present with an aneurysm found incidentally.
1. Rupture
The features of SAH have already been described in detail; they include sudden onset of headache, vomiting, neck stiffness, loss of consciousness, focal signs and epilepsy. Since the severity of the haemorrhage relates to the patients clinical state and this in turn relates to outcome, much emphasis has been placed on categorising patients into 5 level grading systems, e.g. Hunt and Hess.
2. Compression from Aneurysm
A large internal carotid artery aneurysm (or anterior communicating artery aneurysm) may compress.
3. Incidental Finding
The improved availability of sensitive high quality, non-invasive MR or CT imaging techniques has greatly increased the number of patients in whom an intracranial aneurysm is detected incidentally, during investigation for other disease.
Complications of Aneurysmal
INTRACRANIAL
EXTRACRANIAL
- Myocardial infarction
- Cardiac arrhythmias
- Pulmonary oedema
- Gastric haemorrhage (stress ulcer)
Braner Clinics is a professional corporation, and was established for the practice of chronic pain management in 1990. Pain Management is the specialty of Pain Medicine for the assessment, diagnosis and care of severe, chronic persistent pain conditions. Call Now for Quick Appointment: 1 (877) 573-1282