Clinical Features and Treatment of Osteoporosis:
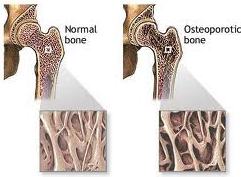 Osteoporosis is characterised by abnormal reduction in bone mass per unit volume, due to poor formation of organic protein matrix. The total bone mass is diminished but the bone present is qualitatively normal. Osteoporosis results because the rate of bone resorption is higher than that of bone formation. There occurs marked reduction in the mechanical strength of the bone and makes the bone vulnerable for fractures following a trivial trauma.
Osteoporosis is characterised by abnormal reduction in bone mass per unit volume, due to poor formation of organic protein matrix. The total bone mass is diminished but the bone present is qualitatively normal. Osteoporosis results because the rate of bone resorption is higher than that of bone formation. There occurs marked reduction in the mechanical strength of the bone and makes the bone vulnerable for fractures following a trivial trauma.
Osteoporosis is a disease of the elderly. It is seen more commonly in females.
Types of Osteoporosis
Osteoporosis can be categorised into two types.
- Primary
- Secondary
Primary osteoporosis
- Type I-postmenopausal osteoporosis: In females, the hormonal changes at menopause cause rapid loss of trabecular bone and result into generalised osteoporosis. These patients became susceptible to fractures of the vertebrae, neck of femur and distal radius.
- Type II-senile osteoporosis: This affects men and women over 60 years of age.
Secondary osteoporosis
A variety of conditions/factors can cause osteoporosis secondarily. These can be broadly classified as:
1. Endocrinal
- Cushing’s syndrome
- Hyperthyroidism
2. Nutritional
- Malnutrition
3. Drug induced
- Prolonged cortisone use
4. Immobilisation
- In fractures
- Bed-ridden patients
5. Miscellaneous
- Cancer disease
- Multiple myeloma
Clinical Features
- The patient presents with backache and pain in the bones.
- The patient gradually develops progressive kyphosis of the dorsal spine.
- More commonly, the patients present with a fracture of neck of femur or the distal radius.
- On examination, there is diffuse tenderness over the spine and other bones generally.
- However, the tenderness may be localised over the spine if there is a pathological compression fracture of the vertebrae.
- There is some decrease in the height due to kyphosis.
Treatment
The mainstay of the treatment is prevention of osteoporosis and measures to increase the bone density, thereby reducing the risk of fractures.
1. Good nutritious diet: This is important because malnutrition and dietary deficiencies are associated with osteoporosis.
2. Exercise: A good level of physical activity acts as an important stimulus to the skeleton; and disuse, immobilisation or denervation paralysis results in bone loss. Physical exercise for 45 minutes at least four times a week helps in increasing the bone mass.
3. Calcium: It has been seen that intake of additional calcium may reduce the bone loss, particularly in postmenopausal women. The recommended dose is 1000 to 1500 mg/day.
4. Vitamin D: Deficiency of vitamin D is commonly seen in the elderly and leads to secondary hyperparathyroidism with resultant bone loss. It helps in the absorption of calcium from the gut.
5. Hormone replacement therapy (HRT): In postmenopausal osteoporosis, HRT reduces the incidence of vertebral and hip fractures.
6. Selective oestrogen receptor modulation (SERM) is a newer class of agent which has effects similar to those of low doses of oestrogen. Raloxifene is a commercially available SERM which is generally well tolerated with a decreased incidence of breast cancer; unlike HRT.
7. Calcitonin: Calcitonin is a peptide hormone secreted by the C-cells of thyroid. It directly inhibits bone resorption. It is known to reduce the incidence of fractures by improving the bone mass. It is administered by injections, but nowadays intranasal preparations are also available.