Investigations, Management And Treatment of Vascular Malformations: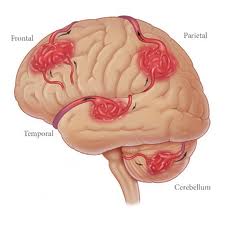
Vascular malformations vary in size and different forms exist:
Arteriovenous malformations (AVMs) are developmental anomalies of the intracranial vasculature; they are not neoplastic despite their tendency to expand with time and the descriptive term ‘angioma‘ occasionally applied.
Dilated arteries feed directly into a tangled mass of blood vessels of varying calibre; they bypass capillaries and shunt oxygenated blood directly into the venous system. Due to high intraluminal pressure, veins may adopt an ‘aneurysmal’ appearance. Arteriovenous malformations occur at any site but are commonest in the middle cerebral artery territory.
- Capillary Telangiectasis: An area of dilated capillaries, like a small petechial patch on the brain surface – especially in the pons. These lesions are often only revealed at autopsy.
- Cavernous Malformation/Angioma: Plum colored sponge-like mass composed of a collection of blood filled spaces with no intervening brain tissue. No enlargement of feeding or draining vessels.
ARTERIOVENOUS MALFORMATIONS
CLINICAL PRESENTATION
- Haemorrhage: About 40 60% of patients with an AVM present with haemorrhage -often with an intracerebral or intraventricular component. In comparison with saccular aneurysms, AVMs tend to bleed in younger patients, i.e. 20-40 years, and are less likely to have a fatal outcome. Vasospasm and delayed ischaemic complications rarely develop. Small AVMs, those with high intranidal pressure and those draining exclusively to deep veins have an increased risk of haemorrhage.
1) Annual Risk of Haemorrhage: Patients with no history of haemorrhage have an annual risk of bleeding of 2-4%. For those presenting with haemorrhage, the risk of re-bleeding may be higher, particularly in the first year. One study reported an annual risk of 17%.
2) Mortality from Haemorrhage: In contrast to the high mortality following aneurysm rupture, haemorrhage from an AVM carries the relatively low mortality rate of approximately 10%.
- Epilepsy: Generalized or partial seizures commonly occur in patients with arteriovenous malformation, especially if the lesion involves the cortical surface. Of patients presenting with haemorrhage, 30% have a history of epilepsy.
- Neurological Deficit: Large AVMs, especially those involving the basal ganglia, may Present with a slowly progressive dementia, Hemiparesis or visual field defect, Probably as a result of a ‘steal’ effect. The infrequent brain stem AVM may also produce a motor or sensory deficit, with or without cranial nerve involvement.
- Headache: Attacks of well localized headache – unilateral and throbbing – occur in a Proportion of patients subsequently shown to have a large AVM.
- Cranial Bruit: Auscultation, especially over the eyeball, occasionally reveals a bruit.
INVESTIGATIONS
- CT scan: Most AVMs are evident on CT scan unless masked by the presence of an intracranial haematoma. A double dose of intravenous contrast may aid visualization, especially with small cryptic lesions.
- MRI: Conventional MRI will clearly demonstrate the AVM as a region of flow voids, with associated signal change within or around the lesion from areas of old haemorrhage or gliosis. The MRI provides exact anatomical detail and helps surgical Planning. Functional MRI aids identification of any adjacent eloquent areas.
- Angiography: Both CT and MR angiography should confirm the presence of an AVM but digital subtraction four-vessel angiography is required to delineate the feeding and draining vessels. Occasionally small AVMs are difficult to detect and only early venous filling may draw attention to their presence.
- N.B.: In the presence of a haematoma, digital subtraction angiography should be delayed until the haematoma resolves, otherwise local pressure may mask demonstration of an AVM. If the angiogram is subsequently negative, then MRI is required to exclude the presence of cavernous malformation.
MANAGEMENT
Various methods of treating arteriovenous malformations are available. All risk further damage and a team comprised of the neurosurgeon and neuroradiologist should decide on the optimal method or combination of methods for each patient. The urgency of the patient’s clinical condition and the risks of treatment must be weighed against the risk of a conservative approach.
Indications for Intervention
- Expanding haematoma associated with AVM
- Progressive neurological deficit
- Risk of haemorrhage especially
- young patients with many years at risk
- AVMs < 3 cm
METHODS OF TREATMENT
- Operation: Excision – complete excision of the AVM (confirmed by per- or postoperative angiography) is the most effective method of treatment particularly for small AVMs in non-eloquent areas. Image guidance may aid localization. Larger lesions (> 6 cm) have a greater risk of postoperative hyper perfusion syndrome and brain swelling and carry a 40% risk of permanent neurological deficit.
- Stereotactic Radio-Surgery: Focused beams from multiple cobalt sources or from a linear accelerator (25Gy) obliterates about 75% of AVMs < 3 cm in diameter, but this may take up to 3 years during which time the risk of haemorrhage persists. In smaller lesions < 1 cm the obliteration rate with 25Gy approaches I0O%. For lesions greater than 3 cm, the lower dose required to minimize the damaging effect of local tissue destruction, makes obliteration unlikely. Pre-treatment with embolisation helps only if this produces a segmental reduction in size. Suboptimal embolisation may merely hinder radio surgical treatment. Despite the delay in action, radio surgery may prove ideal for small deeply seated lesions.
- Embolisation: Skilled catheterization permits selective embolisation of feeding vessels with isobutyl-cyanoacrylate, although this technique is not without risk. Embolisation may cure up to 40% of AVMs when small particularly if supplied by a single feeding vessel, but filling may persist from collaterals. When used preoperatively, it may significantly aid operative removal.
If you are being affected from vascular malformation in the brain disease come instantly Braner Pain Clinic. For more detailed information Call Now: 1 (877) 573-1282